Wound Care: Advanced Healing for Complete Recovery
December 17, 2025 2025-12-17 15:49Wound Care: Advanced Healing for Complete Recovery
The Definitive Guide to Advanced Home Wound Care and Circulatory Health Management Devices
Executive Summary: The Continuum of Home Care Devices for Advanced Wound Care and Vascular Health
The effective management of chronic wounds and complex vascular disorders represents a significant contemporary challenge in healthcare, demanding precise, integrated therapeutic strategies that frequently transition from specialized clinic settings to the patient’s home environment. Achieving optimal healing success requires addressing not only the immediate tissue deficit but also the underlying systemic issues, with circulatory compromise being a frequent and critical factor. This expert analysis details the clinical necessity, functional mechanisms, and optimal application of contemporary home care devices ranging from specialized advanced dressings and Negative Pressure Wound Therapy (NPWT) systems to sophisticated compression modalities and preventative diabetic footwear all designed to optimize healing outcomes and substantially improve patient quality of life. The field of Wound Care has advanced significantly, moving away from outdated methodologies toward evidence-based, moist healing environments and proactive preventative measures. This report serves as a detailed guide to these modalities, emphasizing their mechanism of action and practical application in the home setting.
Section 1: The Modern Science of Wound Management and Healing
1.1. Evolving Paradigms: The Clinical Imperative of Moist Wound Care
The historical practice of exposing wounds to air and allowing them to form a rigid, dry scab has been definitively superseded by the principle of moist Wound Care. This foundational paradigm shift was catalyzed by early discoveries, such as Dr. George D. Winter’s finding that superficial acute wounds healed twice as fast in a moist environment compared to healing under a dry scab. This principle forms the core of modern wound management protocols, as research consistently demonstrates that a controlled moist environment offers significant clinical advantages over the antiquated dry method.
Biological Mechanisms and Accelerated Healing

A controlled moist environment is essential throughout the complex biological cascade that constitutes the healing process, encompassing the inflammatory, proliferative, and maturation stages. During the crucial proliferative stage, moisture actively prevents the wound from drying out, which is vital for reducing pain and minimizing the risk of infection. The presence of moisture enhances critical cellular activities: it acts as an active biological lubricant and metabolic facilitator, supporting the essential migration of specialized cells, such as fibroblasts and keratinocytes, which are crucial for generating new tissue, closing the wound, and facilitating re-epithelization. This enhanced cellular mobility and activity are directly correlated with accelerated healing rates compared to dry methods. The presence of moisture has been proven to facilitate the healing process by enhancing angiogenesis (new blood vessel formation) and collagen synthesis, alongside increasing the breakdown of dead tissue and fibrin.
Furthermore, moist healing prevents catastrophic cellular consequences such as tissue dehydration and cell death that can occur rapidly under a rigid, dry scab. The final stage of healing, the maturation phase, involves the remodeling of newly formed tissue. Maintaining controlled moisture levels during this period supports organized collagen formation, which minimizes disorganization, leading to reduced scarring and a more cosmetically appealing outcome. Clinical studies have concluded that healing in a moist environment results in less inflammation than in a dry environment, thereby improving the overall quality of healing with less scarring.
Functional and Patient Comfort Benefits
Patient comfort is also significantly improved through moist Wound Care protocols. Adequate hydration prevents nerve endings in the wound bed from drying out and becoming hypersensitive, thereby reducing discomfort. The cushioning effect provided by moist dressings protects against external mechanical irritation. Perhaps most critically for adherence to long-term Wound Care protocols, dressing changes are significantly less painful and traumatic. Unlike traditional dry dressings that may adhere to and tear delicate newly formed tissue, modern quality moist wound dressings release easily, ensuring trauma-free changes. Since dry healing remains an entrenched cultural belief for minor injuries, comprehensive patient education must forcefully advocate this evidence-based approach, emphasizing its double benefit of accelerated clinical outcomes and improved patient comfort and compliance.
1.2. Strategic Selection of Advanced Wound Dressings: A Guide to Exudate Management
Effective home Wound Care requires a dynamic strategy of fluid balance control, necessitating the use of specialized dressings chosen based on accurate assessment of the wound type and the level of fluid or exudate it is producing. The optimal home Wound Care kit is not defined by a single product, but by a flexible system of dressings designed to meet the constantly shifting needs of the healing wound bed. This mandates that medical suppliers offer a modular suite of products alongside clear guidance tailored to dryness, heavy exudate, or localized infection.
1.2.1. Hydrocolloids, Hydrogels, and Film Dressings
For wounds with low or minimal exudate, or those requiring rehydration, specific dressings are employed strategically.
- Hydrocolloid Dressings: These utilize gel-forming agents, such as sodium carboxymethylcellulose, typically layered on a semi-permeable film. Upon contact with wound fluid, the agent forms a hydrophilic gel, which serves two primary functions: it rehydrates the wound bed to promote healing, and it facilitates autolytic debridement the body’s natural, gentle enzymatic removal of necrotic tissue. Hydrocolloids are typically intended for wounds with low to moderate exudate, though thin versions are highly beneficial for dry wounds or those with minimal fluid loss. They provide critical protection against friction and shear forces, helping to reduce the risk of a pressure injury forming. Owing to their robust nature and longer wear time, hydrocolloid dressings work effectively under compression bandages, making them suitable for venous leg ulcers.
- Hydrogels: These are primary dressings specifically formulated to manage wound dryness by providing essential moisture and hydration to the wound bed, preventing desiccation. Hydrogels are also recommended for the initial management of small superficial burns after first aid treatment.
- Film Dressings: These transparent, thin, semi-permeable membranes are the simplest form of occlusive dressing. They are best suited for clean wounds without exudate, such as covering surgical suture lines or small superficial burns. They provide a microbial barrier while allowing oxygen exchange.
1.2.2. High-Capacity Management: Foams and Alginates
For heavily draining wounds, high-absorbency products are necessary to prevent maceration of the surrounding skin, maintain an optimal environment, and sustain effective Wound Care.
- Foam Dressings: Often made of polyurethane, foam dressings are highly absorbent and provide valuable cushioning. They are generally recommended for handling moderate levels of exudate. In the strategic context of diabetic foot Wound Care, silicone foam dressings are often specified for moderate exudate levels.
- Alginate Dressings: Derived from natural seaweed components (calcium alginate), these dressings possess superior absorbency compared to foams, making them the preferred choice for managing substantial or high exudate levels. Alginates are also valued for their haemostatic properties; they can be applied as a primary dressing under a secondary foam dressing for actively bleeding wounds.
1.2.3. Specialized Dressings: Antimicrobial Agents in Wound Care
Infection control is paramount in chronic Wound Care, where bioburden and biofilm formation can halt the healing process.
- Silver: Silver-containing dressings deliver a broad-spectrum antibacterial barrier. They are crucial for preventing or managing localized infection and are frequently integrated into protocols for high-risk patients, such as those with diabetic foot ulcers.
- Medical Honey: Medical-grade honey contributes to healing through multiple mechanisms: high osmolarity, high acidity, and the release of hydrogen peroxide. Unidentified phytochemical factors, particularly those found in Manuka honey, contribute non-peroxide-dependent antimicrobial effects. The clinical evidence suggesting that combining medical honey with silver dressings does not diminish the antibacterial effect, and may even enhance it, indicates a potent synergistic strategy for mitigating chronic wound challenges. The osmosis aids in disrupting the biofilm matrix, while the silver provides broad-spectrum bactericidal action.
- Iodine-Based Dressings: Iodine rapidly penetrates microorganisms, damaging proteins and enzymes. However, the use of iodine has declined due to concerns over possible toxic effects. Iodine may be absorbed through large wounds or during prolonged usage, carrying a potential risk of interactions (e.g., hypothyroidism) for patients on medications like lithium.The comparative safety profile strongly favors the use of silver or medical honey products for continuous, non-professional home Wound Care applications.
Table 1: Advanced Wound Dressing Selection Guide by Exudate Level
| Dressing Type | Key Composition/Mechanism | Indication (Exudate Level) | Primary Function in Wound Care |
| Hydrogel | Water or Glycerin-based gel | Dry wounds, minimal exudate, minor burns | Hydration, autolytic debridement |
| Hydrocolloid | Gel-forming agents (CMC) on film | Low to moderate exudate, fragile skin | Occlusion, autolytic debridement, protection |
| Foam (Silicone or Polyurethane) | Highly absorbent polymers | Moderate to high exudate, minor cut/laceration | Absorption, cushioning, moisture retention |
| Alginate | Calcium/Sodium alginate fibers | High to substantial exudate, bleeding wounds | High absorption, hemostasis, gelling |
| Antimicrobial (Silver/Honey) | Active ion release, osmotic effect | Infected or high-risk chronic wounds, odor control | Bioburden reduction, infection barrier, debridement |
1.3. Negative Pressure Wound Therapy (NPWT) Devices: Accelerating Complex Wound Care at Home
Negative Pressure Wound Therapy (NPWT), also referred to as Vacuum-Assisted Closure (VAC), is an advanced adjunctive treatment that has become highly effective for chronic and complex wounds, increasingly transitioning to the monitored home setting. NPWT utilizes a sealed foam dressing and a pump to create suction (subatmospheric pressure) over the wound bed.
Mechanism of Action and Clinical Efficacy
The application of negative pressure (typically $-50$ to $-200\ \text{mm Hg}$) produces a quadruple effect on the wound environment:
- Drainage of Fluids: The system effectively removes excess extracellular fluid and bacteria, which significantly decreases edema (swelling). Less fluid translates directly to reduced tissue tension and improved localized perfusion.
- Macrodeformation: The pressure causes the wound to compress, reducing the size of the cavity and accelerating contraction by approximately 80%.
- Microdeformation: The continuous suction generates mechanical shear and deformation forces on the cells. This cellular stimulation actively promotes angiogenesis (blood vessel formation) and tissue granulation.
- Stabilization: The vacuum assures stability in the environment surrounding the wound, maintaining the necessary clean, moist conditions.
NPWT is effective across various chronic wounds, including pressure ulcers and chronic venous ulcers. Its role in diabetic Wound Care is particularly profound. High-quality meta-analyses confirm that NPWT is a safe and highly effective adjunctive therapy for Diabetic Foot Ulcers (DFUs). The highest-quality evidence shows that NPWT significantly improves healing rates and, critically, decreases major amputation rates (Risk Ratio = 0.69) relative to conventional therapy. This reduction in amputation rates positions NPWT as an indispensable tool for limb salvage in advanced diabetic management.
New modalities enhance the system’s flexibility. NPWT with Instillation (NPWTi-d) combines suction with intermittent delivery of topical solutions for infected wounds. Furthermore, selecting specific foam types, such as the less adherent WHITEFOAM, allows for specialized Wound Care on fragile tissues, minimizing trauma during dressing changes.
Practical Home NPWT Management and Troubleshooting
Successful application in the home requires adherence to specific protocols, primarily maintaining an airtight seal, as failure to do so compromises the therapeutic benefit. Home NPWT devices incorporate advanced alarm systems, underscoring the necessity of patient training on troubleshooting common issues.
- Leak Alarms: A significant leak triggers an alarm, threatening to stop therapy. Resolution involves meticulous inspection, using leak detection procedures (e.g., Seal Check™), ensuring the suction pad is located in a flat area, and minimizing adhesive tape application on the pad itself. For larger, highly exudating wounds, adjusting the intensity to the highest level can facilitate a faster draw down and seal acquisition.
- Low Pressure/Blockage Alarms: These indicate that the system has not reached the prescribed negative pressure. Active steps include checking the tubing for kinks, crimps, or closed clamps. It is essential to ensure that a quarter-sized (2.5 cm) hole has been precisely cut in the drape where the suction pad is placed, as smaller holes can cause blockages and functionality issues. Additionally, lowering the therapy unit and tubing to or below the wound level can help maintain pressure.
- Battery Management: The system provides a critical alarm when only 30 minutes of battery power remains, requiring immediate connection to power. Home users are typically advised to recharge the unit at least twice daily to avoid therapeutic interruption.
Section 2: Compression Therapy and Devices for Optimized Circulatory Health
Compression therapy is the fundamental intervention for addressing circulatory impairment, which is often the underlying cause of many chronic Wound Care problems, such as venous leg ulcers.
2.1. Understanding Venous Dynamics: The Pathophysiology of Chronic Venous Insufficiency (CVI)
Chronic Venous Insufficiency (CVI) is a progressive condition encompassing pathological changes, including lower extremity edema and trophic skin changes, resulting from venous hypertension. The primary cause is the failure or incompetence of venous valves, allowing blood to pool in the legs. If left untreated, CVI progresses, leading to severe complications, most notably venous ulcers (VLUs).
The Mechanical Correction of Compression
 Compression therapy is the cornerstone of conservative CVI and VLU Wound Care management. It achieves its therapeutic effect by mechanically reducing the negative hydrostatic forces associated with venous hypertension.
Compression therapy is the cornerstone of conservative CVI and VLU Wound Care management. It achieves its therapeutic effect by mechanically reducing the negative hydrostatic forces associated with venous hypertension.
- Vascular Support: Compression physically narrows the diameter of the veins, which helps restore competence to residual venous valves, reduces venous reflux, and lowers overall ambulatory venous pressure.
- Tissue Enhancement: By reducing pressure, compression accelerates capillary flow, lowers fluid leakage, and alleviates limb edema. This reduction in swelling is critical because it removes external pressure on the wound bed and surrounding capillaries, thereby improving oxygenation and nutrient delivery to the affected area, encouraging tissue regeneration and faster Wound Care healing. Compression also helps to soften hardened skin (lipodermatosclerosis) and improves both lymphatic flow and function.
The rationale for compression is that it is a pathophysiological intervention
it actively stabilizes the compromised microcirculation, creating a necessary biological environment for healing to proceed successfully.
2.2. Medical-Grade Compression Stockings: Principles and Prescribing
Compression stockings are precisely engineered medical devices that apply calibrated pressure to the limbs.
The Engineering of Graduated Pressure
The design is based on the principle of graduated pressure: the highest compression pressure is applied at the ankle, systematically decreasing toward the knee or thigh. This mechanical gradient efficiently assists the venous system in overcoming gravity, supporting the valves, and moving blood efficiently back toward the heart, preventing pooling.
Compression Classification and Clinical Indications
Compression levels are categorized by pressure measured in millimeters of mercury (mmHg):
- Class 1 (Low Pressure: <20 mmHg): Used for managing mild pain and swelling, and for DVT prevention in low-risk scenarios.
- Class 2 (Medium Pressure: 20–30 mmHg): Used for treating varicose veins, managing moderate venous edema, and often prescribed as the initial therapeutic step for venous conditions and ulcers.
- Class 3 (High Pressure: 30–40 mmHg or higher): Utilized for managing severe, established CVI, post-thrombotic syndrome, and active, complicated venous ulcers, forming the backbone of therapeutic vascular Wound Care.
A critical consideration is the management of patients with mixed arterial and venous pathology (mixed ulcers). In cases where Peripheral Arterial Disease (PAD) is present (ABPI 0.6–0.8), high compression is dangerous. Clinicians must apply modified compression, typically using stiff materials at reduced pressures (less than $40\ \text{mm Hg}$) under careful monitoring, to ensure that venous function is improved without critically impeding already compromised arterial blood flow.
Practical Patient Guidance: Donning Aids and Strategies for Optimal Compliance
The efficacy of compression stockings depends entirely on consistent, daily patient adherence. Compliance is often the greatest therapeutic bottleneck due to the physical difficulty of donning the taut, precise garments, especially for elderly patients or those with comorbid joint issues.
- Adherence Protocols: Stockings should be donned first thing in the morning when limb edema is lowest. The use of specialized accessories, such as rubber gloves (to provide grip and protect the material) and dedicated donning/doffing aids (like the Juzo Easy Fit or Arion aids), are viewed as essential components of the therapy, simplifying the challenge of putting on the garment.
- Fit Integrity: It is vital to pull and spread the fabric in stages, ensuring the material is distributed evenly across the leg. Patients must avoid pulling the material upwards in one go, which can lead to wrinkling and localized constriction that compromises the graduated pressure and can be harmful. Regular fit checks by a medical specialist are necessary to ensure the therapeutic pressure remains accurate over time.
2.3. Intermittent Pneumatic Compression (IPC) Devices and Leg Massagers
Intermittent Pneumatic Compression (IPC) devices, known by various terms including Sequential Compression Devices (SCDs) or therapeutic leg massagers, provide mechanical, dynamic assistance for circulatory health in the home setting.
Sequential Inflation Mechanics and Therapeutic Applications
IPC devices use sleeves containing multiple air bladders that inflate sequentially, starting distally (ankle) and moving proximally up the leg in a coordinated pressure gradient. This mechanical action effectively mimics the physiological calf muscle pump, moving blood toward the heart and promoting the natural release of substances that help prevent clot formation.
- DVT Prevention: IPC is clinically proven for prophylaxis against Deep Vein Thrombosis, especially in patients with reduced mobility.
- Lymphedema Management: IPC pumps, particularly multichamber segmented units, are used when conservative therapies fail. When integrated with complete decongestive therapy (CDT), they significantly enhance lymphedema reduction. Pressure should not exceed $40\ \text{mm Hg}$, and usage is generally restricted to one hour per day under therapist guidelines.
- Venous Ulcer Healing: IPC accelerates VLU healing and controls persistent edema that standard compression stockings may not manage effectively. This advanced adjunct therapy is especially useful for patients with restricted mobility and, crucially, can enhance arterial blood flow in addition to reducing venous pressure, providing a dynamic solution for complex vascular pathology.
2.4. Orthopedic Support Braces: Stability and Indirect Circulatory Benefits
Braces function primarily as joint stabilization devices, but their design provides crucial, indirect support to localized circulatory health and general Wound Care recovery.
- Compression and Edema Control: Many support braces, including ankle and knee supports, integrate gentle compression materials. This localized pressure helps prevent and reduce swelling (edema), which in turn diminishes pain and enhances blood flow to the injured or stressed area, accelerating tissue repair. By managing swelling, braces create a better environment for local perfusion.
- Mobility and Functional Support: Braces stabilize joints, ensuring correct alignment and minimizing detrimental movement. This stability enables patients to safely participate in rehabilitation exercises, maintaining the functional integrity of the muscle pump system that supports venous return.
- Fit Concerns: A critical note involves fit integrity: evidence shows that improperly placed straps or overtightened braces can abnormally elevate intramuscular pressure beneath the compression points, potentially decreasing local muscle blood flow and oxygenation, leading to premature fatigue.
Section 3: Specialized Diabetic Foot and Ulcer Protection
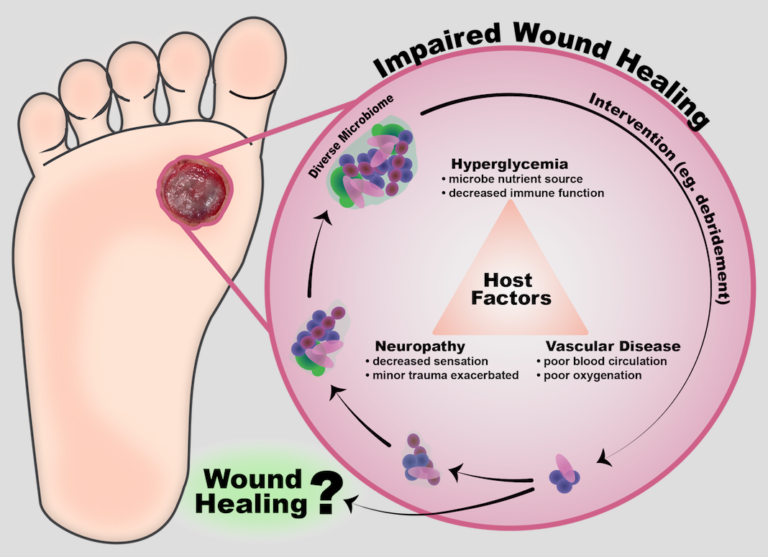
The Diabetic Foot Ulcer (DFU) is a devastating, yet highly preventable, complication of diabetes, requiring rigorous and specialized Wound Care and preventative measures.
3.1. Addressing the Etiology of Diabetic Foot Ulcers (DFUs)
DFUs are precursors to 85% of diabetes-related amputations, establishing diabetes as the leading cause of non-traumatic lower extremity amputations in the U.S.. Approximately 15% of diabetic individuals develop an ulcer, and a high percentage of those necessitate amputation due to resulting complications like bone infection.
Pathophysiological Drivers: Neuropathy, Ischemia, and Stress
DFUs typically arise from the synergistic effects of several underlying pathologies:
- Diabetic Peripheral Neuropathy (DPN): The primary issue is the loss of protective pain sensation, leading to minor trauma and pressure points going unnoticed until severe tissue damage occurs. Furthermore, this lack of pain sensation reduces the patient’s motivation to adhere to prescribed offloading devices, which exacerbates DFU chronicity.
- Peripheral Arterial Disease (PAD): Compromised circulation results in tissue ischemia, which severely delays DFU Wound Care and increases the risk of escalating infection.
- Mechanical Stress: Abnormal biomechanical stress, specifically elevated vertical pressure and shear forces exerted during walking, is the direct initiator for approximately 50% of DFU development.
Because the root causes are identifiable and manageable, foot ulceration is considered arguably the most preventable of all diabetes-related complications. Prevention mandates regular diabetic foot screening and prompt offloading intervention.
3.2. The Essential Role of Offloading and Protective Footwear
Offloading, the practice of diminishing high plantar tissue stress, is the most crucial mechanical intervention for DFU healing and prevention.
Therapeutic Offloading Options for Active Ulcers
- Total Contact Cast (TCC): This remains the gold standard for healing active DFUs, reliably providing consistent results by distributing weight evenly across the entire foot.
- Irremovable Cast Walkers (iTCCs): These are less complicated alternatives to traditional TCCs. Evidence indicates that when removable cast walkers (RCWs) are rendered irremovable, they match the clinical effectiveness of TCCs, often at lower cost and potentially greater convenience.
- Removable Cast Walkers (RCWs): While offering convenience, RCWs suffer from poor compliance; patients frequently remove them for comfort, which compromises the offloading goal and reduces healing efficacy compared to irremovable devices.
Protective Footwear for Long-Term Prevention
For ongoing prevention after ulcer closure, specialized therapeutic protective shoes are essential, especially in patients with biomechanical deformities (e.g., hindfoot varus or valgus). This footwear significantly reduces the incidence of DFU recurrence.
Overcoming Compliance Challenges in Protective Footwear
Patient adherence is the main determinant of success in prevention. Therapeutic footwear often faces significant hurdles related to perception and practicality:
- Aesthetic and Social Barriers: Participants in studies frequently report struggles with consistently wearing therapeutic footwear due to concerns about their appearance, social perceptions, and constraints imposed by workplace dress codes. This tension between medical necessity and professional/social acceptability is a major barrier to effective prevention.
- Strategies for Improvement: Practitioners must provide extensive patient education explaining the whys behind the prescription. Manufacturers have a critical role in addressing this public health challenge by designing better-looking shoes that minimize the aesthetic penalty of therapeutic footwear, ensuring comfort, correct fit, and maximizing adherence.
3.3. Antimicrobial Dressings and Topical Creams in DFU Management
Managing infection is a critical component of specialized diabetic Wound Care.
Targeted Dressings: DFUs require a primary antimicrobial dressing (e.g., silver) coupled with an appropriate secondary absorbent dressing selected based on the exudate level (e.g., silicone foam for moderate drainage).
Topical Antimicrobial Agents: Topical creams and ointments are essential for controlling localized infection and reducing bioburden:
- Clinical Agents: Fusidic acid is utilized for its ability to penetrate intact and damaged skin effectively. Metronidazole is commonly applied to manage the odor associated with anaerobic infections, enhancing patient quality of life.
- Antibiotic Stewardship: For mildly infected DFUs, topical antimicrobial compounds (such as pexiganan) can provide effective treatment comparable to oral systemic antibiotics. This topical strategy is vital for antibiotic stewardship, as it avoids the selection of resistant bacteria associated with broad-spectrum systemic antibiotic use, promoting better long-term infection control for routine Wound Care.
Table 3: Topical Antimicrobial Agents for Local Wound Infection Control
| Agent/Formulation | Mechanism of Action | Key Advantage in Wound Care | DFU Relevance |
| Fusidic Acid (Cream, Gel) | Broad-spectrum (Gram-positive) | Penetrates intact skin, crust, and cellular debris effectively | Local treatment of skin and soft tissue infections |
| Metronidazole (Cream, Gel) | Anaerobic coverage | Reduces odor associated with anaerobic infections (malodorous wounds) | Improving quality of life and managing chronic wounds |
| Medical Honey | High osmolarity, H2O2 production, non-peroxide factors | Autolytic debridement, broad-spectrum antimicrobial activity | Effective for chronic wounds, non-interfering with silver dressings |
| Topical Antibiotics (e.g., Pexiganan) | Targets microbes locally | Avoids selection of systemic antibiotic resistance for mild infections | Strategy for antibiotic stewardship in DFU management |
Section 4: Comprehensive Protocols, Monitoring, and the Future of Home Wound Care
4.1. Patient Empowerment: Protocols for Home Wound Care Assessment
Effective home Wound Care depends on the consistent and accurate monitoring provided by the patient or caregiver, guided by initial training from a licensed healthcare professional.
Critical Monitoring Indicators and Clinical Acumen
Caregivers must be proficient in assessing basic wound metrics, including dimensions, wound base characteristics, and exudate amount. Immediate provider notification is mandatory if key indicators of complication, such as increased pain, increased drainage, or a change in color or odor, are observed.
An important piece of clinical acumen that supports home management is the ability to differentiate inflammation from infection. The simple elevation test elevating the leg for 3 to 5 minutes can suggest venous congestion (vasculitis) if the erythema resolves, helping the caregiver or clinician decide if urgent systemic antibiotic therapy is truly warranted, or if compression adjustments are more appropriate.
The Role of Nutritional Support in Healing
The wound healing cycle is highly energy-dependent, requiring increased caloric intake, protein (up to $1.25–1.5\ \text{g/kg/day}$ for at-risk patients), fluid, Vitamin A, Vitamin C, and Zinc to fuel cellular proliferation and collagen production. Nutritional assessment is therefore an essential part of chronic Wound Care evaluation.
Chronic wound healing failure is often a cascade failure resulting from systemic weaknesses (malnutrition), local impairment (poor circulation), and mechanical disruption (lack of offloading). Therefore, while nutritional optimization is necessary, the 2019 International Working Group on the Diabetic Foot advises against prioritizing nutritional interventions over established standard Wound Care protocols for DFUs, due to limited specific high-quality evidence. A holistic management plan must integrate mechanical and systemic support equally.
4.2. Innovations Shaping Future Wound Care and Home Monitoring
The next generation of advanced home Wound Care is moving toward technology that offers predictive diagnostics and enhanced regenerative capabilities.
Wearable Smart Dressings for Early Detection
These intelligent, flexible systems incorporate sensors for non-invasive, continuous, real-time monitoring of biochemical markers directly at the wound site. This technology fundamentally shifts Wound Care from a reactive model to a predictive one.
- Physiological Markers: Key parameters monitored include pH (a shift toward alkalinity is an early indicator of infection) and temperature (monitoring the $30^\circ\text{C}$–$40^\circ\text{C}$ range).
- Clinical Utility: The capability to monitor subtle changes in pH and temperature allows for the detection of infection in its early stage, providing objective, actionable data that minimizes reliance on subjective human assessment (e.g., odor, pain change). Early detection facilitates rapid, targeted intervention (e.g., adding a topical antimicrobial), reducing the need for systemic antibiotics and preventing complication escalation.
Bioengineered Skin Substitutes for Complex Closure
For chronic wounds that have stalled, bioengineered skin substitutes are increasingly utilized. These materials range from Class I temporary dressings to complex Class III dermal–epidermal composites.
Their function is active regeneration: they act as scaffolds, recruiting essential cells (fibroblasts, keratinocytes) and immune cells, which then secrete crucial cytokines and growth factors. This stimulation promotes angiogenesis, matrix deposition, and re-epithelialization. The availability of advanced Class III products, such as Dermal Regenerative Template (DRT), for specialized home health services represents a major step toward resolving previously refractory chronic ulcers by forcing the wound past the inflammatory phase and into a successful remodeling stage.
4.3. Conclusions: An Integrated Approach to Home Wound Care and Recovery
The demand for specialized, high-level home Wound Care is growing, driven by advancements in medical device technology and robust clinical evidence. Success in managing chronic wounds and circulatory compromise is achieved through an integrated approach that leverages technology to provide clinical-grade treatment outside of the hospital environment.
The principles of moist healing must guide all dressing choices, ensuring that exudate levels are managed dynamically with specific products like hydrocolloids for low exudate or alginates for high exudate, often augmented with antimicrobial components (silver or honey) to manage bioburden.
Vascular health is inextricably linked to Wound Care outcomes. Compression therapy, delivered via medically graded stockings or automated IPC devices, provides necessary mechanical support to reverse the effects of CVI, control edema, and improve local perfusion.
For diabetic limb preservation, the combination of specialized Wound Care protocols, including NPWT devices for complex defects, and meticulous long-term offloading through prescribed therapeutic footwear, is proven to accelerate healing and significantly reduce amputation risk. Manufacturers have a responsibility to address patient adherence barriers by prioritizing product comfort and appearance.
The future of Wound Care is characterized by convergence merging advanced mechanical therapies (NPWT, IPC) with real-time digital monitoring (smart dressings) and regenerative materials (skin substitutes). By offering this continuum of high-quality, evidence-based devices, comprehensive and proactive management is achieved, ensuring optimal healing outcomes and a definitive pathway to recovery for patients managing chronic conditions at home. Visit our shop here, and for any more questions contact us here.