Conquer Sleep Apnea: 5 Treatments for Better Sleep!
August 4, 2025 2026-01-14 9:40Conquer Sleep Apnea: 5 Treatments for Better Sleep!
Conquering the Night: A Comprehensive Guide to Sleep Apnea Treatment and Better Sleep with Turquoise Medical
Introduction: Unmasking the Silent Struggle of Sleep Apnea
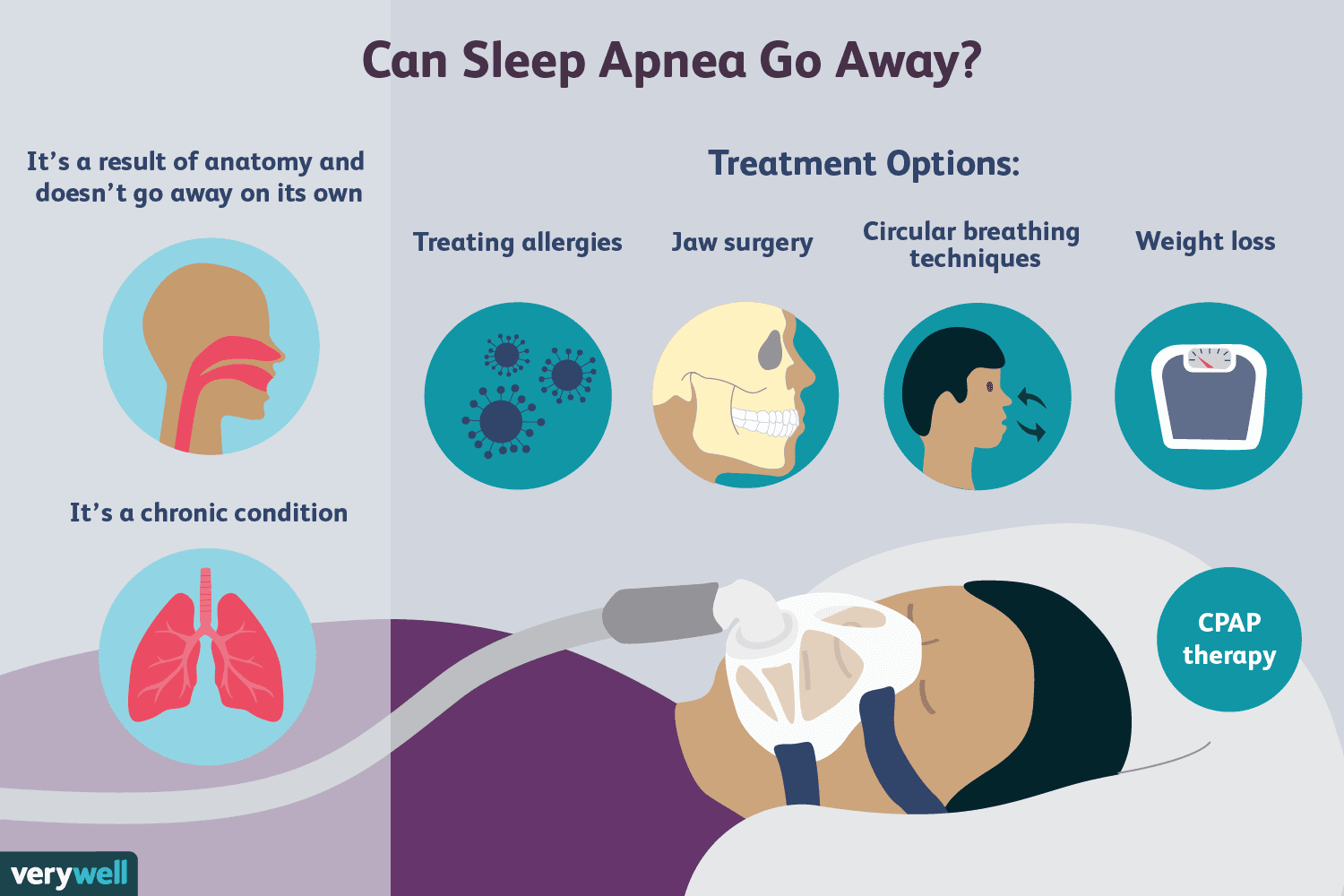
Sleep apnea represents a significant and often underdiagnosed chronic sleep disorder characterized by recurrent interruptions in breathing during sleep.1 These pauses, which can occur numerous times throughout the night, profoundly impact an individual’s health and daily functioning, underscoring the critical importance of understanding and effectively addressing this condition. The pervasive nature of sleep apnea, coupled with its potential for severe health consequences, necessitates a clear understanding of its different forms and available management strategies.
The condition is primarily categorized into two distinct types: Obstructive Sleep Apnea (OSA) and Central Sleep Apnea (CSA). Obstructive Apnea is the more prevalent form, arising when the muscles in the throat relax excessively during sleep. This relaxation causes the upper airway to narrow or completely collapse, leading to brief cessations of breathing.
In contrast, Central Apnea is less common and results from the brain’s temporary failure to transmit appropriate signals to the muscles responsible for breathing, leading to a lack of respiratory effort.Distinguishing between these two types is fundamental for accurate diagnosis and tailored management.
Untreated sleep apnea is recognized as a serious medical condition with far-reaching health implications. The intermittent oxygen deprivation and fragmented sleep associated with the disorder can contribute to a cascade of health problems, ranging from cardiovascular complications to cognitive impairment. Therefore, timely diagnosis and effective treatment are paramount to mitigating these risks and fostering overall well-being.
In the pursuit of improved respiratory and sleep health, Turquoise Medical stands as a dedicated partner, offering advanced solutions designed to address the complexities of sleep apnea. The organization is committed to providing high-performance respiratory devices and comprehensive sleep apnea solutions for both homecare and hospital environments.6 Their role extends to supporting patients with essential sleep apnea medical devices within their homes, integrating these solutions into a broader framework of comprehensive healthcare facility support.6 This commitment underscores their dedication to empowering individuals to achieve restorative sleep and better health outcomes.
Understanding Sleep Apnea: Symptoms, Causes, and Risk Factors
A thorough understanding of the indicators and origins of sleep apnea is crucial for early recognition and timely intervention, paving the way for effective sleep apnea treatment.
Recognizing the Signs: Common Sleep Apnea Symptoms
Identifying the observable signs of sleep apnea is often the first step towards diagnosis. These symptoms can be broadly categorized based on when they manifest, helping individuals or their loved ones pinpoint potential issues.
Nighttime Symptoms: These are the signs typically observed during sleep, often by a bed partner. The most frequently reported symptom is loud, disruptive snoring, which is a common indicator of partial airway obstruction.Beyond snoring, individuals may exhibit gasping, choking, or snorting sounds as their airway struggles to reopen.7 A critical sign is witnessed breathing pauses, where a bed partner observes periods when breathing stops entirely.7 Other nocturnal indicators include restless sleep, characterized by tossing and turning, frequent urination during the night, and consistent mouth breathing.7
Daytime Symptoms: The impact of fragmented sleep extends significantly into waking hours, manifesting as various daytime symptoms. Excessive daytime sleepiness, or hypersomnia, is a hallmark symptom and the most common medical cause of severe drowsiness.5 This can lead to individuals falling asleep unintentionally during monotonous activities such as reading, watching television, or, critically, while driving, which substantially increases the risk of work-related and motor vehicle accidents.
Despite seemingly adequate sleep duration, individuals with sleep apnea often wake up feeling unrefreshed.7 Morning headaches, which can persist for hours and occur on most days, are also common.7 A dry or sore throat upon waking is frequently experienced due to consistent mouth breathing during sleep.7 The chronic sleep deprivation can also lead to cognitive impairment, including difficulties with memory, impaired intelligence, attention deficits, and an increased likelihood of making errors.7 Furthermore, mood changes, such as irritability, depression, and anxiety, are frequently observed.5 A decreased interest in sex or impotence may also be reported.5
The detailed symptom list, separated by night and day, serves as a practical guide for self-identification or recognition by loved ones. The emphasis on witnessed snoring or apnea highlights the crucial role bed partners often play in the initial detection of the condition. This observation frequently serves as the primary impetus for seeking a professional sleep apnea diagnosis. By presenting these symptoms comprehensively, the report empowers individuals to consider a medical evaluation, understanding that the effects of sleep apnea extend far beyond sleep itself, impacting cognitive function, mood, and even safety.
Table: Key Sleep Apnea Symptoms (Daytime & Nighttime)
| Symptom Category | Specific Symptom |
| Nighttime Symptoms | Loud, Disruptive Snoring |
| Gasping, Choking, or Snorting | |
| Witnessed Breathing Pauses (Apnea) | |
| Tossing and Turning during sleep | |
| Frequent Urination | |
| Mouth Breathing while sleeping | |
| Daytime Symptoms | Excessive Daytime Sleepiness (Hypersomnia) |
| Waking Up Tired/Unrefreshed | |
| Morning Headaches | |
| Dry or Sore Throat upon waking | |
| Cognitive Impairment (memory, attention, errors) | |
| Mood Changes (irritability, depression, anxiety) | |
| Decreased Sex Drive/Impotence |
Unraveling the Roots: Sleep Apnea Causes and Risk Factors
Understanding the underlying physiological mechanisms and identifying the various factors that increase an individual’s susceptibility to sleep apnea is essential for both prevention and targeted sleep apnea treatment.
The fundamental cause of Obstructive Sleep Apnea lies in the relaxation of throat muscles during sleep, which leads to a narrowing or complete collapse of the upper airway.7 This obstruction forces the individual to exert greater effort to inhale against a closed or constricted passage, resulting in reduced oxygen levels, increased carbon dioxide, and fragmented sleep.7
Several factors significantly increase the likelihood of developing sleep apnea:
- Excess Weight/Obesity: This is a predominant risk factor, as fatty deposits around the upper airway can physically obstruct breathing.1 Even a moderate amount of weight loss can significantly alleviate airway constriction.1 Medical conditions associated with obesity, such as hypothyroidism and polycystic ovary syndrome, can also contribute to the risk.5
- Older Age: The risk of obstructive sleep apnea generally increases with age, typically leveling off after the 60s and 70s.5
- Narrowed Airway/Anatomical Features: A naturally narrow airway can be an inherited trait, or it may be caused by enlarged tonsils or adenoids that block the airway.5 Specific physical features such as a small or recessed lower jaw (retrognathia), an enlarged tongue base, or a neck circumference larger than 17 inches are also significant anatomical risk factors.7
- Male Sex: Men are generally two to three times more likely to develop OSA than premenopausal women. However, the risk substantially increases for women after menopause.5
- High Blood Pressure (Hypertension): Obstructive sleep apnea is notably common in individuals with hypertension.5
- Chronic Nasal Congestion: Persistent nasal congestion, regardless of its underlying cause (e.g., allergies), can double the risk of OSA.5 Addressing and treating underlying allergies can be beneficial.1
- Smoking: Individuals who smoke are up to three times more likely to have OSA, as smoking can cause inflammation and swelling in the upper airway.1
- Diabetes: Sleep apnea is more prevalent in individuals with diabetes and can exacerbate diabetes-related complications.5
- Family History of Sleep Apnea: Having immediate family members with OSA increases an individual’s risk, potentially due to shared anatomical features, lifestyle patterns, or environmental factors.5
- Asthma: Research indicates an association between asthma and an increased risk of obstructive sleep apnea.5
The interconnectedness of various sleep apnea risk factors, such as obesity leading to a narrowed airway which is further exacerbated by smoking and congestion, suggests that sleep apnea is often a manifestation of broader systemic health issues rather than an isolated condition. This understanding emphasizes the importance of a holistic approach to sleep apnea treatment, integrating lifestyle modifications with medical interventions.
Identifying these risk factors allows for targeted screening and early intervention, which can potentially mitigate future complications. While some factors like a naturally narrow airway or family history indicate inherent predispositions, highlighting modifiable risk factors reinforces that lifestyle changes are not just supplementary but integral to effective treatment plans, setting the stage for discussions on comprehensive management strategies.
Table: Common Sleep Apnea Risk Factors
| Risk Factor | Description/Impact |
| Excess Weight/Obesity | Fat deposits around the upper airway can obstruct breathing; a leading cause of OSA. |
| Older Age | Risk increases with age, typically leveling off after 60s/70s. |
| Narrowed Airway/Anatomical Features | Inherited trait or caused by enlarged tonsils/adenoids; includes small jaw, large tongue base, large neck circumference. |
| Male Sex | Men are 2-3 times more likely than premenopausal women; risk increases in women after menopause. |
| High Blood Pressure (Hypertension) | Sleep apnea is common in individuals with high blood pressure. |
| Chronic Nasal Congestion | Persistent congestion can double the risk of OSA. |
| Smoking | Increases OSA risk by causing inflammation and swelling in the upper airway. |
| Diabetes | More prevalent in individuals with diabetes; can worsen diabetes complications. |
| Family History of Sleep Apnea | Increased risk due to shared anatomical features, lifestyles, or environment. |
| Asthma | Research indicates an association with increased risk of OSA. |
The Diagnostic Journey: Sleep Apnea Test and Diagnosis
While recognizing sleep apnea symptoms is a crucial first step, an accurate sleep apnea diagnosis necessitates a thorough evaluation by a qualified medical professional, typically a sleep specialist. Self-diagnosis is insufficient for effectively managing this complex condition.
The diagnostic process typically commences with a detailed clinical history. During this stage, the physician will inquire about the patient’s symptoms, sleep patterns, and any observations reported by bed partners.10 This is followed by a physical examination to identify predictive features such as obesity, an enlarged neck circumference, retrognathia (posterior chin position), or a narrow oropharyngeal opening.10 Screening questionnaires, such as the STOP-Bang tool, may be utilized to assess the risk of Obstructive Sleep Apnea, though their accuracy for a definitive diagnosis can be limited.10
Polysomnography (Sleep Study): The Gold Standard
Polysomnography (PSG), commonly referred to as a sleep study, is considered the definitive and “gold standard” sleep apnea test for diagnosing sleep apnea.10 This comprehensive test is typically conducted overnight in a specialized sleep laboratory, where the patient’s sleep is monitored by an attendant.10 PSG collects data from multiple physiological channels, providing a detailed picture of sleep architecture and respiratory events.
These channels include an electroencephalogram (EEG) to monitor brain waves for sleep staging, an electrooculogram (EOG) for eye movements, an electromyogram (EMG) for muscle activity, an electrocardiogram (ECG) for heart activity, and various respiratory channels to track airflow, breathing effort, and oxygen levels.10 Both full-night studies, primarily for diagnosis, and split-night studies, where diagnosis and positive airway pressure titration occur in the same night, can be performed.10
Home Sleep Apnea Tests (HSATs): An Alternative
For certain patients, particularly those with a high pretest probability of moderate to severe Obstructive Sleep Apnea, Home Sleep Apnea Tests (HSATs) offer a convenient alternative.10 While HSATs can be effective in identifying high-risk individuals, they are generally considered less accurate than in-lab PSG (Type-I studies). This reduced accuracy stems from fewer monitored channels and the inability of HSATs to differentiate between sleep and wakefulness, which can lead to an estimated rather than a precise Apnea-Hypopnea Index (AHI).10 Additionally, data loss due to detached or malfunctioning monitoring equipment is a potential limitation.10
Understanding the Apnea-Hypopnea Index (AHI)
The Apnea-Hypopnea Index (AHI) is the key metric derived from a sleep apnea test and is crucial for diagnosis. It is calculated by summing the total number of apneas (complete airflow obstructions) and hypopneas (partial airflow obstructions) that each last for a minimum of 10 seconds. This sum is then divided by the total sleep time in hours.10 Hypopneas are specifically measured by a 3% or more oxygen desaturation or an arousal from sleep.10 The diagnostic criteria for Obstructive Sleep Apnea typically involve an AHI of 15 or more events per hour, or 5 or more events per hour when accompanied by associated symptoms like daytime sleepiness or cardiovascular comorbidities.10
The detailed explanation of diagnostic methods, particularly the nuanced discussion of polysomnography versus home sleep apnea tests and the importance of the Apnea-Hypopnea Index, demonstrates a deep medical understanding. This level of detail helps manage patient expectations regarding the diagnostic process and empowers them to comprehend the clinical basis for their sleep apnea diagnosis, which is an essential prerequisite before initiating any sleep apnea treatment. The entire diagnostic journey is presented as a crucial foundation, as without an accurate diagnosis, appropriate interventions cannot be prescribed.
Comprehensive Management: Sleep Apnea Treatment Options
CPAP Therapy: The Cornerstone of Sleep Apnea Treatment

Continuous Positive Airway Pressure (CPAP) therapy is widely recognized as the most common and often the first-line sleep apnea treatment for Obstructive Sleep Apnea.8
Mechanism of Action and Benefits: A CPAP machine functions by drawing in room air, filtering and pressurizing it, and then delivering a continuous flow of this pressurized air through a tube into a mask worn over the nose or both the nose and mouth.8 This constant positive pressure gently keeps the upper airway passages open throughout the entire respiratory cycle, effectively preventing the collapse of the tongue, uvula, and soft palate. This action halts snoring and prevents sleep apnea events.8
The immediate benefits of consistent CPAP use are significant and often quickly noticeable. Patients typically report improved sleep quality, feeling more rested upon waking, a reduction or complete elimination of snoring, and a marked decrease in daytime sleepiness (hypersomnia).8 Many individuals also experience enhanced concentration, memory, and overall cognitive function, alongside an improved mood.8 Beyond these immediate improvements, CPAP therapy offers crucial long-term benefits, including a reduced risk of serious health issues. This encompasses a lower risk of cardiovascular disease events such as heart attack, stroke, and high blood pressure, as well as improved blood pressure control and alleviation of pulmonary hypertension.8
Types of PAP Machines and Their Functionalities: Several types of positive airway pressure (PAP) devices are available, each with specific mechanisms and applications:
- CPAP (Continuous Positive Airway Pressure): This is the most basic type, administering a single, constant level of pressure to maintain an open airway during both inhalation and exhalation.13 It is generally the most affordable and has a simpler design, often serving as the initial therapy for OSA.13 Some models incorporate a pressure relief setting to slightly lower pressure during exhalation, enhancing comfort.14
- APAP (Auto-Adjusting Positive Airway Pressure) / Auto-CPAP: These are more advanced devices that automatically adjust the air pressure level within a prescribed range in real-time, based on the patient’s breathing patterns.13 This auto-adjusting technology can detect changes in breathing due to factors like sleeping position or varying obstruction severity, increasing or decreasing pressure accordingly. An APAP machine may not require a titration study to determine optimal pressure settings, as it adapts dynamically.13
- BiPAP (Bilevel Positive Airway Pressure) / BPAP: This machine delivers two distinct pressure levels: a higher pressure during inhalation (inspiratory positive airway pressure, IPAP) and a lower pressure during exhalation (expiratory positive airway pressure, EPAP).8 BiPAP machines are often prescribed for individuals with more complex or severe breathing issues, or for those who find the constant pressure of a CPAP machine difficult to tolerate.14 They can operate in various modes, including spontaneous, spontaneous-timed, or timed modes, and some offer pressure support ventilation (PSV) to help regulate breathing rate and volume.13 Auto-BiPAP variants also exist, offering auto-adjusting capabilities for both inhalation and exhalation pressures.13
- ASV (Adaptive Servo-Ventilation): This is a specialized PAP device primarily utilized for certain types of central sleep apnea. ASV continuously monitors the patient’s breathing and adjusts pressure levels to stabilize breathing patterns, even delivering a breath if necessary to ensure consistent respiration.8
- Travel CPAP Machines: These are compact, portable versions of standard CPAP devices, specifically designed for ease of travel. They allow patients to maintain their CPAP therapy consistently, even when away from home, ensuring continuity of treatment.13
Table: Comparison of PAP Machine Types
| Machine Type | Function/Mechanism | Primary Use Case/Recommendation | Approximate Cost Range |
| CPAP | Consistent air pressure level for breathing in and out. | Most common initial therapy for Obstructive Sleep Apnea (OSA). | $500-$1,000 13 |
| APAP | Auto-adjusting level of air pressure that is generally the same for inhalation and exhalation, adapting to breathing patterns. | Moderate to severe OSA; for sleepers whose needs change throughout the night. | $600-$1,600 14 |
| BiPAP | Delivers two distinct pressure levels: higher for inhalation, lower for exhalation. | More complex or severe breathing issues; for patients who cannot tolerate CPAP. | $1,700-$3,000 14 |
| ASV | Monitors breathing and adjusts pressures to stabilize breathing; can deliver a breath when necessary. | Certain types of Central Sleep Apnea. | (Cost not specified in snippets) |
| Travel CPAP | Portable version of CPAP, offering same therapeutic benefits. | Portability and ease of use for travel. | $450-$1,200 14 |
Mask Types and Considerations for Comfort and Adherence: The choice and proper fit of the mask are paramount for both the effectiveness and comfort of CPAP therapy. Various mask types cater to different patient needs and preferences:
- Nasal Mask: This option covers the entire nose and is often recommended for individuals who tend to move frequently during sleep.8
- Nasal Pillow Mask: Rather than covering the entire nose, this mask features cushions or prongs that fit directly into the nostrils, covering only the nostril area. This design allows for comfortable wearing of glasses.8
- Full Face Mask: A triangular mask that fits over both the nose and mouth, making it ideal for individuals who breathe through their mouth during sleep or who have nasal blockages.8
- Hybrid Mask: A type of full face mask that covers the mouth and seals the nostrils with prongs or cushions, without covering the bridge of the nose.8
The optimal mask choice depends on individual face shape, sleeping position, and breathing habits (whether primarily nasal, oral, or both).1 It is worth noting that most CPAP accessories, including masks, are universally compatible with different machine types.14
Addressing Common Side Effects and Solutions: While the benefits of CPAP therapy are substantial, initial adjustment can be challenging, and some common side effects may arise. However, practical solutions are available to mitigate these issues. Dry mouth, nasal congestion, a runny nose, or nosebleeds are common issues often caused by the dry air delivered by the machine. The use of a heated humidifier, which is frequently integrated into the CPAP machine or available as an accessory, can significantly alleviate these symptoms by moistening the air.1 Skin irritation or redness can result from mask pressure or an improper fit.
Ensuring the correct mask size, achieving a proper but not overly tight seal, and utilizing adequate padding can prevent pressure sores and irritation. For individuals who find it difficult to fall asleep with high pressure, many PAP devices offer a “pressure ramp” feature. This setting starts at a lower, more comfortable pressure for the first 5 to 45 minutes and gradually increases to the prescribed therapeutic level as the patient drifts off to sleep.13
Poor tolerance and compliance can be initial hurdles; the first few times using a CPAP machine may be difficult.8 However, early patient education and ongoing support are crucial factors that significantly improve adherence rates.10 In rare hospital settings, mild sedation may be considered to improve compliance in agitated or delirious patients, always under close medical monitoring. The detailed breakdown of PAP machine types, mask options, and practical solutions for common side effects highlights a deep understanding of the patient experience beyond just the medical mechanism.
This approach positions Turquoise Medical as a client-focused provider, recognizing the nuances of sleep apnea medical devices and the critical importance of patient adherence for successful sleep apnea treatment outcomes. By explaining the various options and solutions, the report implicitly conveys that patients have increasingly comfortable and effective options available, which is a positive message for those considering sleep apnea treatment.
Beyond CPAP: Exploring Other Treatment Avenues
While CPAP therapy is frequently the primary recommendation, it is important to acknowledge that not all patients tolerate it or find it fully effective. For these individuals, alternative and supplementary sleep apnea treatment options, including various surgical interventions and oral appliances, are available.
Surgical Interventions: Surgical approaches for sleep apnea are typically considered for individuals who cannot tolerate or do not achieve sufficient relief from CPAP or other non-surgical methods.15
- Uvulopalatopharyngoplasty (UPPP): This procedure involves the surgical removal of excess tissue from the back of the mouth and the top of the throat (palate). In some cases, the tonsils and adenoids may also be removed if they are enlarged.9 The goal of UPPP is to enlarge the airway and reduce obstruction.
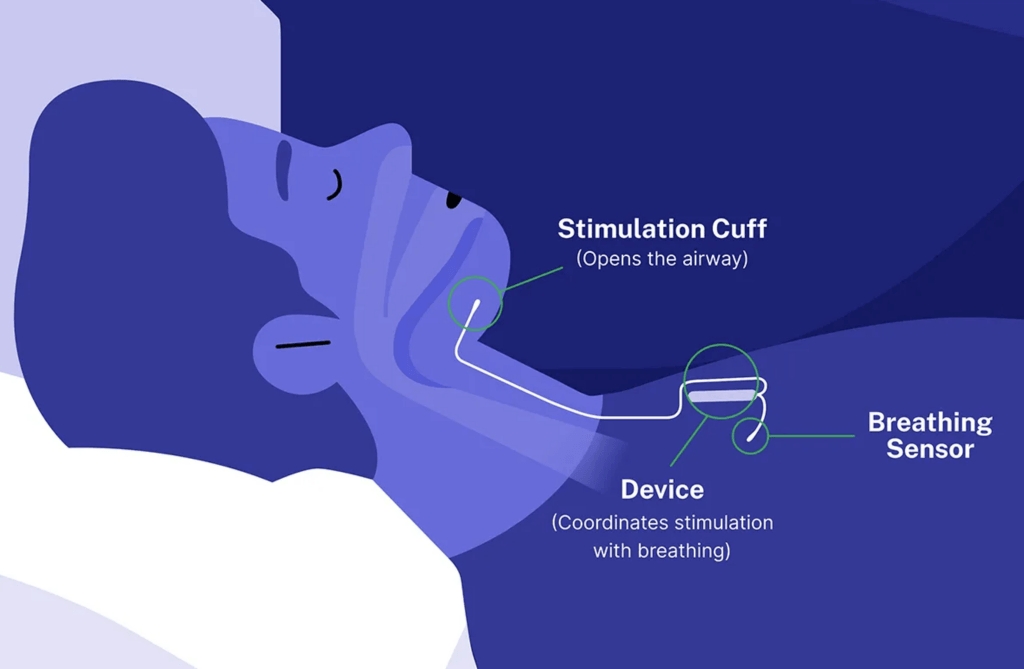
- Upper Airway Stimulation (e.g., Inspire device): This represents a newer, advanced sleep apnea medical device approved for moderate to severe obstructive sleep apnea in patients who cannot tolerate CPAP or BiPAP.9 A small, thin impulse generator, known as a hypoglossal nerve stimulator, is surgically implanted under the skin in the upper chest. When the patient inhales, the device stimulates the nerve that controls tongue movement, causing the tongue to move forward and prevent throat blockage.9 Studies have demonstrated significant improvements in OSA symptoms and overall quality of life with this therapy.9
- Maxillomandibular Advancement (MMA) / Jaw Surgery: In this procedure, the upper and lower parts of the jaw are surgically moved forward relative to the rest of the facial bones. This action significantly enlarges the space behind the tongue and soft palate, thereby making airway obstruction less likely.9
- Tracheostomy: This is a more drastic surgical option, typically reserved for severe, life-threatening obstructive sleep apnea when all other treatments have failed.9 During a tracheostomy, a surgeon creates an opening in the neck and inserts a tube for breathing, effectively bypassing the blocked upper airway.9
- Nasal Surgery: Procedures such as the removal of nasal polyps or straightening a deviated septum (a crooked partition between the nostrils) can help improve airflow through the nasal passages. Improved nasal breathing can contribute to better overall breathing during sleep.9
- Tonsillectomy/Adenoidectomy: Surgical removal of enlarged tonsils or adenoids, particularly common in children, can alleviate airway obstruction caused by these tissues.9 The Sleep Surgery Clinic at Mayo Clinic specializes in these surgical treatments for both adults and children with OSA who have not found relief with other options like CPAP.15
Oral Appliance Therapy: Custom-fitted oral appliances, typically prescribed by dentists with expertise in sleep medicine, can be an effective sleep apnea treatment for mild to moderate OSA. These devices work by repositioning the jaw or tongue forward to keep the airway open during sleep.
Presenting various surgical options beyond CPAP demonstrates a comprehensive understanding of sleep apnea treatment pathways, acknowledging that CPAP is not a universal solution. This approach highlights the depth of medical knowledge and accuracy, reflecting the medical researcher’s perspective, and provides hope for patients who may struggle with CPAP adherence.
The fact that surgical options like Upper Airway Stimulation are approved for those who “can’t tolerate CPAP or BPAP” emphasizes a critical clinical need and offers solutions for non-adherence. Detailing innovative sleep apnea surgery techniques also showcases advancements in sleep apnea medical devices and surgical care, appealing to readers seeking cutting-edge solutions and reinforcing the authoritative tone of the report.
Empowering Yourself: Sleep Apnea Lifestyle Changes
Beyond medical devices and surgical interventions, actionable sleep apnea lifestyle changes can significantly improve symptoms, often complementing medical interventions and forming a crucial part of a holistic sleep apnea treatment plan. These changes empower patients to actively participate in their health management.
- Weight Management: For individuals who are overweight or obese, even moderate weight loss can significantly relieve constriction of the airway.1 Obesity is identified as one of the leading causes of obstructive sleep apnea.8 Adopting a well-balanced diet rich in fruits, vegetables, lean proteins, and whole grains can aid in maintaining a healthy weight. It is also advisable to avoid heavy meals close to bedtime, as they may worsen symptoms.16
- Regular Exercise: Engaging in consistent physical activity, such as aerobic exercise and strength training, can improve overall sleep quality and contribute to weight management.9 The recommendation is to aim for at least 30 minutes of moderate exercise most days of the week.16 It is always prudent to consult a doctor before commencing any new exercise regimen.
- Limit Alcohol and Smoking: Both alcohol consumption and smoking can exacerbate sleep apnea symptoms. Alcohol relaxes the muscles in the throat, potentially leading to increased airway obstruction, while smoking causes inflammation and swelling of the air passages.1 Reducing or eliminating these habits can substantially improve the sleep apnea condition.1
- Positional Therapy: Sleeping on your side or stomach rather than on your back can prevent the tongue and soft palate from resting against the back of your throat and blocking your airway.1 Simple techniques, such as sewing a tennis ball into the back of your pajama top or strategically placing pillows, can help deter rolling onto your back during sleep.1
- Nasal Hygiene: Maintaining open nasal passages during sleep can significantly improve breathing. If experiencing congestion, using a saline nasal spray can be helpful.9 Treating underlying nasal allergies can also be beneficial, as swollen airway tissues make breathing more difficult.1
- Maintain a Consistent Sleep Schedule: Going to bed and waking up at the same time every day, including weekends, helps regulate the body’s internal clock (circadian rhythm) and significantly improves the quality of sleep.1
- Elevate Your Head During Sleep: Utilizing an adjustable bed or wedge pillows to slightly raise the upper body can help keep airways open and reduce the chances of obstruction by the tongue and soft tissues.16
- Avoid Sedatives and Sleeping Pills: While these medications may induce sleep, they can excessively relax throat muscles, potentially worsening sleep apnea symptoms.1 Exploring natural relaxation techniques as alternatives is advisable.
- Create a Sleep-Friendly Environment: Transforming the bedroom into a sanctuary for restful sleep is important. Ensure the room is cool, dark, and quiet to promote relaxation. Investing in a comfortable mattress and pillows that provide adequate support for the head and neck is also beneficial.1
- Mouth Exercises (Oropharyngeal Exercises): Studies suggest that specific exercises targeting the muscles of the mouth, tongue, and face can help improve daytime sleepiness, snoring, oxygen intake, and overall sleep quality in individuals with sleep apnea.1
- Use a Humidifier: Research indicates that humidifiers can be effective in preventing CPAP failure by alleviating dryness and improving patient comfort.1
- Review Prescriptions: Some prescription medications, particularly muscle relaxers and painkillers (especially opioids), can worsen sleep apnea by relaxing the upper airway. It is crucial to discuss all current medications with your doctor.1
- Meditation/Yoga Breathing: Certain yoga breathing exercises and meditation techniques may help improve factors related to sleep apnea, although further studies are needed to fully understand this link.1
The detailed list of sleep apnea lifestyle changes reinforces that sleep apnea treatment is multifaceted and often requires active patient engagement beyond just medical devices. This empowers patients with actionable steps and highlights the importance of a holistic approach to health, which can significantly reduce symptom severity and improve treatment efficacy.
Many of these lifestyle changes directly address underlying sleep apnea risk factors, demonstrating how these modifications can reduce the severity of the condition itself, potentially even leading to remission in some cases. The inclusion of exercise, diet, stress reduction, and sleep environment optimization showcases a comprehensive view of health, emphasizing that sleep apnea is influenced by broader lifestyle choices.
The Broader Impact: Understanding Sleep Apnea Complications
The gravity of untreated sleep apnea cannot be overstated, as it extends beyond mere sleep disruption to encompass a range of potential long-term health consequences. Understanding these sleep apnea complications underscores why timely and effective sleep apnea treatment is critical.
- Daytime Fatigue and Sleepiness: A direct consequence of the lack of restorative sleep at night, individuals with untreated sleep apnea experience severe daytime drowsiness, chronic fatigue, and increased irritability.5 This significantly impairs concentration, attention, and increases the likelihood of making errors.7 Most dangerously, it can manifest as falling asleep at work, while watching television, or, critically, while driving, with people with Obstructive Sleep Apnea being two to three times more likely to be involved in motor vehicle accidents.5 In children and young people, untreated sleep apnea can lead to poor academic performance and behavioral problems.5
- Cardiovascular Problems: The repeated drops in blood oxygen levels (hypoxia) and sudden awakenings during sleep apnea episodes place immense strain on the cardiovascular system. This significantly increases the risk of developing high blood pressure (hypertension), a major risk factor for heart disease.5 The severity of sleep apnea correlates directly with a greater risk of coronary artery disease, heart attack, heart failure, and stroke.5 Furthermore, sleep apnea increases the risk of heart rhythm problems (arrhythmias), which, in individuals with underlying heart disease, can potentially lead to sudden death.5
- Cognitive Impairment: Beyond general fatigue, untreated sleep apnea can lead to more specific cognitive deficits, including impaired memory, reduced thinking abilities, and difficulty with attention and problem-solving.7
- Mental Health Changes: Sleep apnea is strongly associated with various mental health issues, including increased irritability, depression, and anxiety.5 The chronic sleep deprivation and physiological stress inherent to the condition contribute significantly to these mood disturbances.
- Diabetes and Metabolic Syndrome: Individuals with sleep apnea have a higher likelihood of developing insulin resistance, metabolic syndrome, and type 2 diabetes.5 Untreated sleep apnea can also worsen existing diabetes and increase the likelihood of developing diabetes-related complications.7
- Complications with Medicines and Surgery: Sleep apnea poses a significant concern when certain medicines or general anesthesia are administered. Sedatives, some prescription painkillers (especially opioids), and general anesthetics can relax the upper airway muscles, potentially worsening sleep apnea and leading to severe breathing problems.1 Patients with sleep apnea are more prone to complications after major surgery, particularly if sedated and lying on their back.5 It is crucial for patients to inform their surgeon about any known sleep apnea or related symptoms before any surgical procedure.5
- Eye Problems: Some research has identified a connection between obstructive sleep apnea and certain eye conditions, such as glaucoma, although these complications are often treatable.5
- Sleep-Deprived Partners: The loud snoring often associated with sleep apnea can severely disrupt the sleep of bed partners, leading to their own sleep deprivation and potentially straining relationships. Some partners may resort to sleeping in separate rooms to get adequate rest.5
The extensive list of sleep apnea complications reveals that it is not merely a sleep nuisance but a systemic health threat, affecting multiple organ systems and significantly impacting quality of life and safety. This elevates the urgency for sleep apnea treatment and highlights the long-term value of investing in solutions. The complications span cardiovascular, metabolic, neurological, and mental health domains, demonstrating that sleep apnea has far-reaching effects throughout the body, reinforcing the need for comprehensive medical management and underscoring the long-term benefits of sleep apnea medical devices.
The inclusion of sleep-deprived partners and the increased risk of drowsy driving accidents illustrates a deeper understanding of the societal and interpersonal consequences of untreated sleep apnea, broadening the report’s scope beyond individual patient health to public safety and relationship well-being. The specific mention of complications with medicines and surgery, along with the crucial advice to inform surgeons about sleep apnea, provides vital practical medical guidance..
The Connection: Sleep Apnea and Snoring
The relationship between sleep apnea and snoring is often misunderstood. Clarifying this connection is essential, as snoring frequently serves as a key indicator that warrants further investigation for potential underlying sleep apnea.
Snoring is a very common symptom of sleep apnea.When the airway is partially blocked during sleep, the air passing through causes the soft tissues in the back of the throat to vibrate, producing the characteristic snoring sound.This mechanical vibration is a direct result of the obstructed airflow.
It is important to note the high prevalence of snoring among those diagnosed with sleep apnea; approximately 90% of individuals with sleep apnea also snore.This strong association often makes snoring the first observable sign that prompts concern.
However, a crucial distinction must be made: not all snorers have sleep apnea.Many individuals snore harmlessly without experiencing the recurrent breathing interruptions characteristic of sleep apnea. Nevertheless, if snoring is loud, frequent, and accompanied by other concerning signs such as gasping, choking, snorting, or witnessed breathing pauses, it is a strong indicator of potential sleep apnea and warrants a professional medical evaluation.
This distinction is vital to avoid unnecessary alarm for casual snorers while effectively guiding high-risk individuals towards a necessary sleep apnea test. Clarifying this nuanced relationship manages reader expectations and provides a clear, actionable call for those with concerning snoring patterns. Snoring, while often perceived as a mere nuisance, serves as a significant gateway symptom for sleep apnea, frequently observed by a bed partner. Highlighting this connection provides a practical entry point for individuals to consider a serious medical condition and prompt them to seek a sleep apnea test.
Your Partner in Health: Why Choose Turquoise Medical for Sleep Apnea Solutions?
Turquoise Medical stands as a trusted provider of sleep apnea medical devices and comprehensive solutions, aligning with the critical need for reliable support in managing this condition.
Turquoise Medical demonstrates an unwavering commitment to providing advanced respiratory therapy and intensive care solutions, which fundamentally include comprehensive sleep apnea solutions.6 Their dedication focuses on improving patient outcomes through high-quality equipment and robust support systems.
The organization offers a variety of high-performance respiratory devices, including essential sleep apnea medical devices, designed for seamless integration into both homecare and hospital settings.6 This encompasses their capability to support patients with these crucial devices within their homes, as part of their broader commitment to comprehensive healthcare facility solutions.6 While specific product models are not detailed in available information, the emphasis remains on the breadth and quality of their offerings within the sleep apnea domain.
Beyond merely providing equipment, Turquoise Medical is committed to supporting patients throughout their sleep apnea treatment journey. This commitment includes ensuring access to necessary equipment and actively contributing to the effective management of their condition, reflecting a patient-centric approach to care. Despite limitations on specific product details, this section effectively uses available information to position Turquoise Medical as a holistic provider of sleep apnea medical devices and solutions. The focus shifts from individual product features to their broader commitment to patient care and comprehensive solutions, building brand authority and trust.
Individuals seeking reliable sleep apnea medical devices or comprehensive respiratory solutions are encouraged to visit the Turquoise Medical website (https://turquoisemedical.com/) to explore their offerings and learn how they can assist in managing sleep apnea for improved health and quality of life. This serves as a direct and clear call to action, guiding interested readers to the client’s website for more specific information and engagement.
Conclusion: Taking Control of Your Sleep Health
The journey to better sleep and improved health begins with understanding and addressing sleep apnea. This comprehensive guide has detailed the critical importance of recognizing sleep apnea symptoms, seeking a timely and accurate sleep apnea diagnosis through a professional sleep apnea test, and exploring the comprehensive range of sleep apnea treatment options available. These options span from cornerstone CPAP therapy and other advanced sleep apnea medical devices to beneficial sleep apnea lifestyle changes and, in some cases, sleep apnea surgery. The serious nature of sleep apnea complications if the condition is left untreated, highlighting systemic health risks, underscores the urgency of proactive management.
Prioritizing sleep health is a fundamental component of overall well-being. Individuals experiencing symptoms or those at risk are strongly encouraged to consult with healthcare professionals to discuss their concerns, undergo appropriate testing, and develop a personalized sleep apnea treatment plan. Effective management of sleep apnea can lead to significant improvements in energy levels, cognitive function, cardiovascular health, and overall quality of life, transforming the silent struggle into a path towards restorative sleep and better health.
The report’s detailed information, from symptoms and diagnosis to diverse treatment modalities and potential complications, aims to empower individuals with the knowledge necessary to take control of their sleep health. This comprehensive approach, encompassing both medical interventions and self-care strategies, underscores the multifaceted nature of sleep apnea management and the profound positive impact it can have on an individual’s life.



